A.G. Anghel, I. Anghel, M. Dumitru, D. Cristian, T. Burcos
E.N.T. Department, Coltea Clinical Hospital, Bucharest, Romania
Surgery Department,Coltea Clinical Hospital,Bucharest, Romania
Rezumat
Utilizarea gastrostomelor la pacienåii cu neoplazie cervico-facialã
Scop: Inventarierea cazurilor de neoplasm cervico-facial ce au beneficiat de gastrostomã în cadrul Spitalului Clinic Colåea Bucuresti cu evidetåierea similarittåilor si diferenåelor fatã de datele publicate la nivel mondial.
Paciemtii si metode: Am analizat retrospectiv 64 de proceduri de gastrostomã din perioada 2008-2011, efectuate la pacienåi cu neoplazie cervico-facialã.
Rezultate æi discuåii: Grupul nostru de studiu a prezentat numeroase caracteristici specifice (un numãr mai mare de cazuri cu vârsta peste 55 ani decât pacienåi tineri; predominanåa utilizãrii gastrostomiei chirurgicale în defavoarea tehnicilor minim invazive; aproximativ 2/3 din gastrostome au fost efectuate la pacienåi cu carcinom laringian; aproximativ 1/3 din gastrostome au fost instalate pretratament; etc).
Concluzii: 22% din gastrostome au fost efectuate dupã apariåia unei fistule faringocutanate. Astfel vom demara un viitor studiu prospectiv pentru a verifica dacã utilizarea profilacticã a PEG va duce la scãderea apariåiei fistulelor faringocutanate.
Abstract
Purpose: To analyse the gastrostomy procedures performed in HNC patients admitted to Coltea Clinical Hospital in order to underline the similarities and differences to the data published worldwide.
Patients and methods: Our retrospective study contains 64 HNC cases that met the inclusion criteria between 2008 and 2011.
Results and discussions: The study group presents numerous specific characteristics (a larger number of cases aged over 55 than younger patients; elective use of classic gastrostomy instead of newer techniques; approximately two thirds of the gastrostomies were performed in patients with laryngeal carcinoma; only one third approximately of the cases benefited from prophylactic gastrostomy; etc.).
Conclusions: 22% of the gastrostomies were made after the appearance of a pharyngocutaneous fistula. Therefore we will begin a future prospective study in order to ascertain the value of prophylactic PEG in preventing the appearance of pharyngocutaneous fistulas.
Background
One of the major problems in the management of HNC patients is the maintenance of an adequate nutritional status. (1,2,3,4,5)
The treatment course is often complicated by the development of painful mucositis, which causes difficulty in oral intake. (6) Furthermore, in some patients, dysphagia occurring as a result of CRT causes life-threatening aspiration pneumonia during and/or after treatment. (7) These obstacles to oral intake often result in treatment failure, prolongation of hospitalization, and treatment-related death. (8)
Feeding gastrostomies are well-established as a method of providing satisfactory nutritional support and can be inserted percutaneously under direct vision using an endoscope (percutaneous endoscopic gastrostomy) under radiologicalguidance, or using a conventional open/laparoscopic surgical approach. (9,10)
The value of prophylactic PEG tube placement at treatment initiation being increasingly recognized, and evidence suggests that patients experience better outcomes. (11) Criteria for patient selection have not been defined completely, and a great deal of variation in clinical practice exists, contributing to underuse of this supportive intervention. (12,13)
In our institution, newly diagnosed HNC patients scheduled to receive radiation and/or chemotherapy are offered the choice of a gastrostomy before the start of treatment but the majority postpones this procedure until the instalment of treatment-related complications. (14)
Objectives. Materials and Methods
We conducted a retrospective descriptive study comprising the patients submitted to gastrostomy procedures from Colåea Clinical Hospital Bucharest during 2008-2011.
Our study’s objectives are:
1) Descriptive analysis of our study group (gender distribution, age group distribution, morphological types);
2) Analysis of the types of gastrostomy procedures used;
3) Analysis of the timing for performing selective gastrostomies in order to identify preventable complications; Inclusion criteria for our study group:
1) patient with a gastrostomy procedure;
2) histological diagnostic of certainty for HNC;
3) were included only those patients with traceable complete examination charts.
Exclusion criteria for the cases in our study group:
1) patient without a gastrostomy procedure;
2) lack of histological diagnostic of certainty for HNC;
3) only those patients with traceable complete examination charts were included;
Therefore we have identified 64 cases with HNC which benefited from gastrostomy procedures and met the inclusion criteria.
For statistical analysis we have used Microsoft Excel and SPSS. We have crosschecked our data with the General Surgery Department.
Results and Discussions
Our study group numbers 64 patients with gastrostomy procedures (surgical gastrostomy and percutaneous gastrostomy) during 2008-2011 at Colåea Clinical Hospital Bucharest.
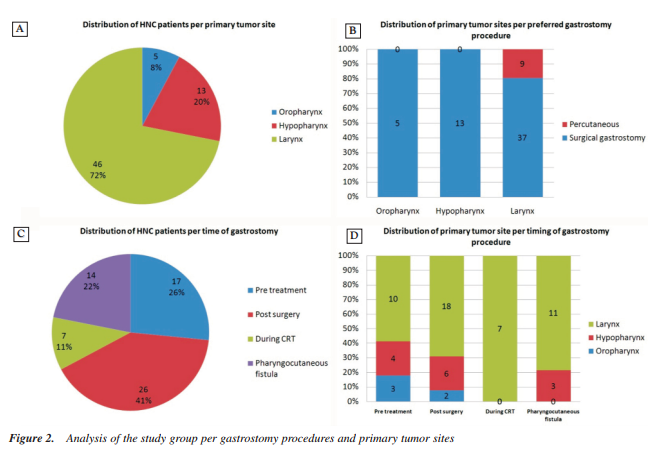
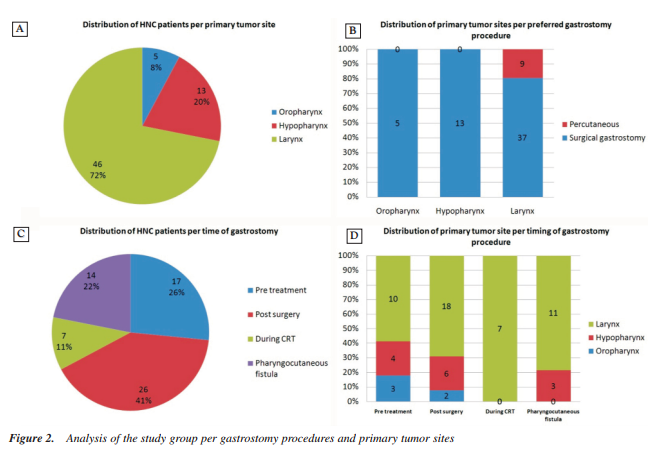
Concerning the sex distribution of the cases in our study group, we observed the male dominance - around 91% of the cases, similarly to worldwide statistics concerning HNC. (Fig. 1A)
There is an urban predominance of the patients with gastrostomy procedures, around 56%. (Fig. 1B) This is mainly because of the greater understanding of the use of a gastrostomy procedure by the better educated urban patients opposed to a feeling of shame and lack of proper care characterizing rural counterparts.
The age group distribution of the HNC subgroup records a maximum number of 27 (42, 18%) patients between 55-64 years. In the areas with high HNC prevalence the evolution in case numbers has a growth in plateau till the 5th decade of age with a sudden fall in number at higher ages. On the contrary inside our study group the age curve has a plateau towards the 6th and 7th decades where we record a higher number of cases than those of young patients. (Fig. 1C)
Concerning the distribution of the study population per gastrostomy procedure we record a predominant use of the surgical classic gastrostomy 55 cases (86%) and very few percutaneous gastrostomy cases 9 (14%). (Fig. 1D)
This aspect may be explained by the fact that in our department few HNC benefit from prophylactic gastrostomies and in the course of treatment other types of gastrostomies become technically challenging or prohibited due to the need to pass suture lines like in the case of total laryngectomies or due to extreme edema of the pharynx or larynx during CRT.
Nevertheless we have financial difficulties in acquiring PEG materials.
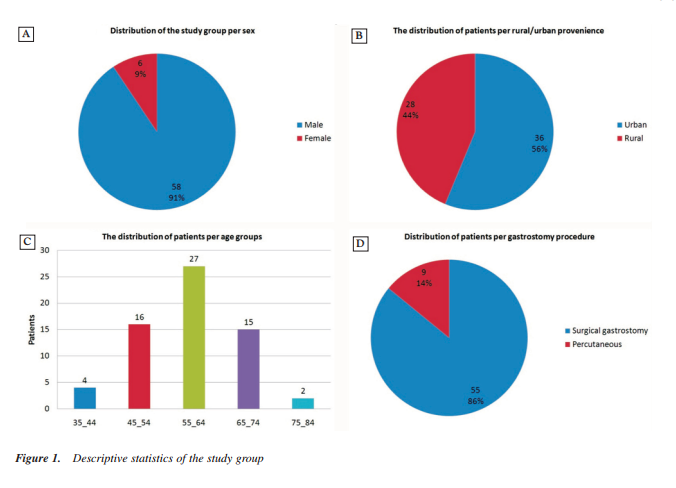
From the point of view of the distribution of HNC caseswith gastrostoma per primary tumor site, there is a majority of 46 cases (72%) with carcinoma of the larynx. A possible explanation for these cases could be the fact that our unit is specialized in the treatment of this pathology and many difficult cases are sent from other regions. (Fig. 2A) Needless to
mention that many of the cases affecting the tongue and oral cavity are sent to OMF specialists and thus we found a small number of patients with carcinoma of the oropharynx.
All the percutaneous procedures were performed in patients with pathology at the level of the larynx. (Fig. 2B)
Although all our patients are offered the possibility of prophylactic gastrostomy, only 26 % accept this procedure before any other treatment. (Fig. 2C) The majority of gastrostomies are performed after the surgical treatment (41%). There are an alarming number of cases with
pharyngocutaneous fistula (22%) due to the late staging of the cases at arrival in our unit.
Moreover, by combining the above data, a patient with carcinoma of the larynx will likely benefit from a gastrostomy procedure after the surgical treatment and that procedure will be a classic one; a patient with carcinoma of the oropharynx willmost likely not be associated with a pharyngocutaneous fistula. (Fig. 2D) Furthermore, the choice of the gastrostomy procedure taking into consideration when the procedure, was performed,shows that percutaneous procedures are used mainly for prophylactic gastrostomies, while the cases with pharyngocutaneous fistula benefit from a surgical approach exclusively.
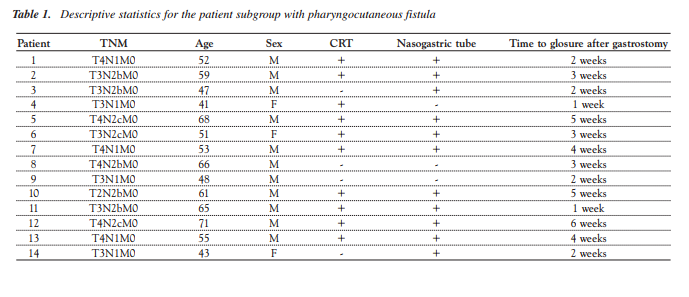
In Table 1 we present the data regarding the subgroup with pharygocutaneous fistula that received gastrostomy. Given the fact that we have a close relationship with the oncology department all the fistulas in this group were diagnosed early, the usual symptom being difficult swallowing followed by the presence of alimentary residues at the level of the tracheotomy cannula. The fistula treatment applied in our department: a gastrostomy procedure followed by watch and wait management until the fistula closes. A fistula is declared closed only after 2 consecutive swallowing tests with methylene blue. One should note the fact that the patients without a nasogastric tube had a quicker resolution of the fistula. The same supposition can be made about the patients who developed the fistula outside the CRT. The majority of patients were fistula free in < 4 weeks after the gastrostomy procedure.
Another important aspect is that from the 17 cases that received a gastrostomy procedure before any other treatment only 1 developed a pharyngocutanous fistula.
Conclusions
The 64-patients study group diagnosed with HNC and having gastrostomy performed on presents numerous characteristics that sustain epidemiologic data such as sex distribution, age group distribution, and histological type distribution.
However there are some specific characteristics for our study group:
- There is a higher number of cases aged over 55 years than younger patients;
- We record a predominant use of the surgical classic gastrostomy, whereas in other countries percutaneous procedures rank first;
- From the point of view of the distribution of HNC cases with gastrostoma per primary tumor site, there is a majority of 46 cases (71,87%) with carcinoma of the larynx;
- Although all our patients are offered the possibility of prophylactic gastrostomy, only 26 % accept this procedure before any other treatment.
- All pharyngocutaneous fistulas closed quicker after the gastrostomy procedure.
- Patients without a nasogastric tube and those who developed the fistula outside the CRT had a quicker resolution of the fistula.
Because 22% of the gastrostomies were made after the appearance of a pharyngocutaneous fistula, we will begin a future prospective study in order to ascertain the value of prophylactic PEG in preventing the appearance of pharyngocutaneous fistulas.
References
1. Ishiki H, Onozawa Y, Kojima T, Hironaka S, Fukutomi A, Yasui H, et al. Nutrition support for head and neck squamous cell carcinoma patients treated with chemoradiotherapy: how often and how long? ISRN Oncol. 2012;2012:274739.
2. Oakley RJ, Donnelly R, Freeman L, Wong T, McCarthy M, Calman F, et al. An audit of percutaneous endoscopic gastrostomy insertion in patients undergoing treatment for head and neck cancer: reducing the incidence of perioperative airway events by the introduction of a tumor assessment protocol Ann R Coll Surg Engl. 2009;91(3):249-54.
3. Cady J. Nutritional support during radiotherapy for head and neck cancer: the role of prophylactic feeding tube placement. Clin J Oncol Nurs. 2007;11(6):875-80.
4. Madhoun MF, Blankenship MM, Blankenship DM, Krempl GA, Tierney WM. Prophylactic PEG placement in head and neck cancer: How many feeding tubes are unused (and unnecessary)? World J Gastroenterol. 2011;17(8):1004-8.
5. Meirovitz A, Kuten M, Billan S, Abdah-Bortnyak R, Sharon A,
Peretz T, et al. Cytokines levels, Severity of acute mucositis and the need of PEG tube installation during chemo-radiation for head and neck cancer - a prospective pilot study. Radiat Oncol. 2010;5:16.
6. Malmgren A, Hede GW, Karlström B, Cederholm T, Lundquist P, Wirén M, et al. Indications for percutaneous endoscopic gastrostomy and survival in old adults. Food Nutr Res. 2011;55.
7. Martin L, Blomberg J, Lagergren P, Patients' perspectives of living with a percutaneous endoscopic gastrostomy (PEG).
BMC Gastroenterol. 2012;12:126.
8. Pang AS. Time for the world to move beyond the percutaneous endoscopic gastrostomy. World J Gastroenterol. 2011;17(23):2877-8.
9. Irinel Popescu. Tratat de chirurgie, vol. VIII A + B, chirurgie generala. Bucuresti: Editura Academiei Române; 2008.
10. Bohannon IA, Carroll WR, Magnuson JS, Rosenthal EL.
Closure of post-laryngectomy pharyngocutaneous fistulae. Head Neck Oncol. 2011;3:29.
11. Palomar-Asenjo V, Sarroca Capell E, Tobías Gómez S, Pérez Hernández I, Palomar-García V.Pharyngocutaneous fistula following total laryngectomy. A case-control study of risk factors implicated in its onset. Acta Otorrinolaringol Esp. 2008;59(10):480-4. Spanish
12. Sarra LD, Rodríguez JC, García Valea M, Bitar J, Da Silva A.Fistula following total laryngectomy. Retrospective study and bibliographical review. Acta Otorrinolaringol Esp. 2009; 60(3):186-9. Spanish
13. Berteşteanu SV, Popescu CR, Grigore R, Popescu B. Pharyngoesophageal junction neoplasia - therapeutic management. Chirurgia (Bucur). 2012;107(1):33-8.
14. Dumitra A, Sabãu A, Maniu D, Grosu F, Smarandache G, Ursache E, et al. Particular aspects of endoprosthesis in malignant advanced pharingeal-esophageal stenosis. Chirurgia (Bucur). 2011;106(3):327-32. Romanian