I. Anghel, A.G. Anghel, M. Dumitru, C.C. Soreanu
E.N.T. Department, Coltea Clinical Hospital, Bucharest, Romania
Rezumat
Carcinomul nazofaringian – analiza factorilor de riscsi a markerilor imunologici
Scop: Inventarierea factorilor de risc asociaåi CNF prezenåi la pacienåii trataåi în cadrul clincii ORL a Spitalului Clinic Coltea Bucuresti cu evidentierea similaritãtilor si diferentelor fatã de datele existente la ora actualã la nivel mondial.
Pacienti si metode: Am analizat retrospectiv 178 de cazuri din perioada 2003-2011 ce au îndeplinit criteriile de includere în cadrul grupului nostru de studiu.
Rezultate si discutii: Grupul nostru de studiu a prezentat numeroase caracteristici specifice (un numãr mai mare de cazuri cu vârsta peste 60 ani decât pacienåi tineri; o scãdere linearã a numãrului de cazuri pentru grupa de vârstã 30-39 ani; aproximativ 1/3 din cazuri nu au prezentat nici un factor de risc; >10% din cazuri au fost asociate cu limfoame, etc.).
Concluzii: Caracteristicile imunohistochimice identificate la pacienåii noştrii cu forme de CNF nediferenåiat sunt: MNF116, CK19, S100,CD34betaE12, Ki67, EBV pozitiv; restul markerilor fiind negativi (CerB2, EGFR, COX2, p53, CK7, CD117, VGFR, PCNA, L26/CD20, UHCL1, CD15, CD30, VIM, TTF1, CLA, CK17, CEA, LMP, CD79a, EMA).
Abstract
Purpose: To analyze the risk factors associated with Nasopharyngeal Carcinoma (NPC)in patients admitted to the ENT Department at Coltea Clinical Hospital in order to assess the similarities and differencesas compared to the epidemiological datainternationally reported.
Patients and methods: This is a retrospective study on 178 cases that met the inclusion criteriafrom 2003 to 2011.
Results and discussions: There are a number of specific characteristics noticed in our study group: a larger number of cases aged over 60 than younger patients; a linear fall in number of the cases aged between 30-39 years; approximately one third of the cases did not have any of the traditional risk factors; more than 10% of the cases were associated with lymphoma, etc.
Conclusions: The immunologic pattern of our patients presenting undifferentiated NPC is the following: MNF116, CK19, S100, CD34betaE12, Ki67, EBV positive. The rest of the markers were negative (CerB2, EGFR, COX2, p53, CK7, CD117, VGFR, PCNA, L26/CD20, UHCL1, CD15, CD30, VIM, TTF1, CLA, CK17, CEA, LMP, CD79a, EMA).
Introduction
Incidence rates for NPC vary enormously among different populations. In endemic areas the numbers can be fifty times higher than in other areas. The highest incidence is found in southern China. In Hong Kong, NPC reaches 30 cases/100.000 men. This disease is 3 times more frequent in men than in women. NPC evolves at a much younger age than other forms of cancer as it has the highest incidence below the age of 50. The incidence rises after the second decade and reaches a plateau for both sexes till the age of 50when it drops gradually. (1)
The development of NPC is the result of a complex interaction between genetic factors, early EBV infection and environmental carcinogens. Genetic susceptibility plays an important role in NPC pathogenesis. HLA alleles such as A2,A33, B46, B58, Cw1 and DR3 are often present in NPC patients. (2) A2, Cw1, B46 haplotype is associated with an earlier age of debut. On the other hand A2 haplotype without B46 or B58 has a better survival rate. (3) The discovery of EBV receptors on pharyngeal epithelial cells has established the connection between EBV and NPC. (4,5) In Hong Kong the incidence for both sexes has dropped rapidly with approximately 30% in the last 20 years but the age distribution pattern has remained unchanged. A possible explanation may be the fact that the individual level of exposure tocarcinogens has dropped but the mechanism of exposure is the same. (6)
Numerous potential agents have been studied including dust, smoke and industrial fumes. NPC incidence in women is still lower than men worldwide despite the growing number of smoking women. (7,8) There has been reported a higher risk of developing NPC in subjects with professional exposure to formaldehyde. (9,10)
Jia et al. (11) analyzed a strong association between NPC and a diet rich in salted fish and poor in vegetables during childhood. Salted fish, which is traditional in southern China contains an important quantity of volatile nitrosamines. These are alkylating agents known to induce malignant tumors in laboratory animals. Dietary carcinogens affect only susceptible populations given the fact that Japan has a low incidence for NPC despite similar consumption of salted fish and canned vegetables.
In Romania, IARC reported an incidence of 1.7% in 100.000 men and 0.85% in 100.000 women for NPC. (12) We cannot attribute these numbers to salted fish consumption, but we can take into consideration the lack of fresh vegetables in basic diet, excessive smoking habits and childhood EBV infection. (13)
The early detection of NPC is almost impossible in our country given the lack of access to the healthcare system; therefore we are still encountering terminal pathologyas in other parts of the globe with a poor economy. (14)
In the light of the above, our patients are treated by radiotherapy primarily, other types of treatment being unsuitable for the stage or too expensive. (15-20)
Materials and Methods Materials and Methods
We conducted a retrospective descriptive study on 178 patients diagnosed with NPC in the ENT Clinic at Coltea Clinical Hospital Bucharest during 2003-2011.
Our study’s objectives are:
1. Descriptive analysis of our study group (gender distribution, age groups distribution, morphological types);
2. Analysis of NPC risk factors impact on the patients (chronic smoking, alcoholism, professional chemical exposure and EBV infection);
3. Immunologicalfeatures of the biopsy material in order to identify certain molecular characteristics with possible prognostic values.
Inclusion criteria for our study group:
1. histological diagnostic of certainty for NPC;
2. if the histologist requested an immunological differential diagnostic toVictor Babes National Research and
Development Institute for Pathology and Biomedical
Sciences, Bucharest we included only the cases which received the results back;
3) we included only the patients with traceable complete examination charts.
Exclusion criteria:
1. lack of histological diagnostic of certainty for NPC;
2. lack of immunologic analysis for those cases which required differential diagnosis;
3. all the cases without traceable or with incomplete examination charts.
Therefore,from a total of 206 cases of NPC admitted to our hospital 28 cases were excluded: 17 did not meet theinclusion criteria and 11 were subsequent admissions of the same patients to different departments in our hospital.
For statistical analysis we used Microsoft Excel and SPSS. In order to correlate the immunological analysis we used the reference materials available on the website www.vbabes.ro.
Results and Discussions Results and Discussions
Our study group included 178 patients diagnosed with NPC during 2003-2011 at Coltea Clinical Hospital Bucharest.
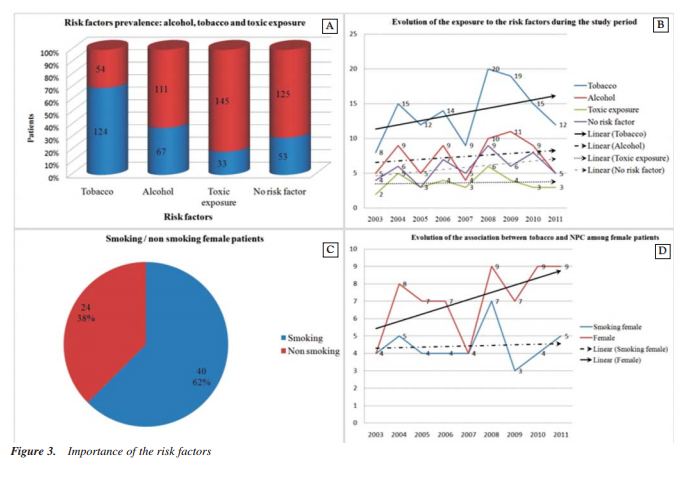
Concerning the sex distribution we observed predominance in male sex with 114 (64%) cases, similarly to worldwide statistics, Fig. 1A.
From 2003 to 2011 we recorded a maximum number of 29 patients (16,29%) in 2008 with a fall in numbers in the following years probably due to the general fall in accessibility to the medical system on the background of the economic crises in the EU. A minimum number of 12 (6,74%) patients with NPC was recorded in 2003.The small number of cases analyzed for the period 2003-2007 isdue to the failure in meetingthe inclusion criteria; Fig. 1B.
We discovered a linear growth in number of cases for both sexes during the study period which confirms the annualgrowth of cases with NPC worldwide, Fig. 1C.
The age groups distribution records a maximum number of 52 (29,21%) patients between 50-59 years. In the areas with high NPC prevalence the evolution in case numbers has a growth in plateau till the 5th decade of age with a sudden fall in number at a higher ages.On the contrary inside our study group the age curve has a plateau towards the 6th and 7th decades where we record a higher number of cases, Fig. 1D.
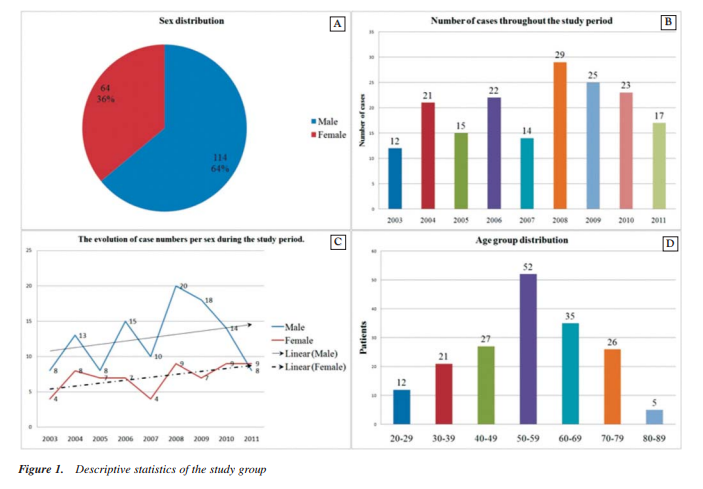
Regarding the evolution in number of cases per age group during the analyzed time frame one can notice a constant linear growth. However there are 2 contradictory situations: the linear fall in case numbers for the 30-39 years age group which can be explained by the longer exposure of these individuals to modern prevention campaigns concerning tobacco use and alcohol consumption; the other contradictory situation is given by the 80-89 years age group which has a constant number of cases throughout the study period, Fig. 2A, 2B.
The histological analysis places theundifferentiated forms of NPC on the first place with 96 (54%) cases.
Although despite the general epidemiological data which considers lymphomas as a minority, there are 20 (11%) cases in our study group. This aspect is probably influenced by the oncology-hematology specific of our hospital, Fig. 2C.
From the histological point of view the evolution in case numbers shows a linear decrease of the cases diagnosed with spindle cell NPC in spite of the general pattern growing in numbers for all NPChistological types. Moreover there is a linear constant evolution for the metastasis of other malignancies at nasopharyngeal level. This aspect is influenced by the diagnostic protocols used by the majority of surgeons and physicians which consider metastatic cases as terminal and refer them to oncology departments without consulting an ENT specialist; Fig. 2D.
The prevalence of risk factors in our study group is the following: tobacco use 124 (69,66%) cases; alcohol consumption 67 (37,64%) cases and professional toxic exposure 33 (18,33%) cases; Fig. 3A. The importance of EBV infection was partially quantified because of the positive identification of the virus. It was realized only for the patients with histological samples needing an immunologicaldifferential diagnosis which was sent to the Victor Babes Institute. The large number of cases without any of the risk factors is alarming: 53 (29,77%). Although a possible explanation for these cases can be the fact that our unit is specialized in the treatment of this pathology and many difficult cases are sent from other regions, one can notice the growing linear number of such cases throughout the study period, Fig. 3B. Furthermore, there are a constant number of cases associated with toxic professional exposure in spite of theclosure of the chemical industry. These cases seem to be part of a reservoir population, which probably will decline in the future.
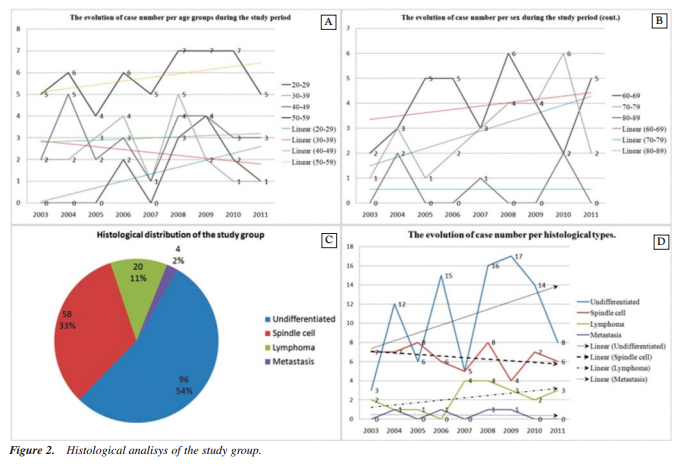
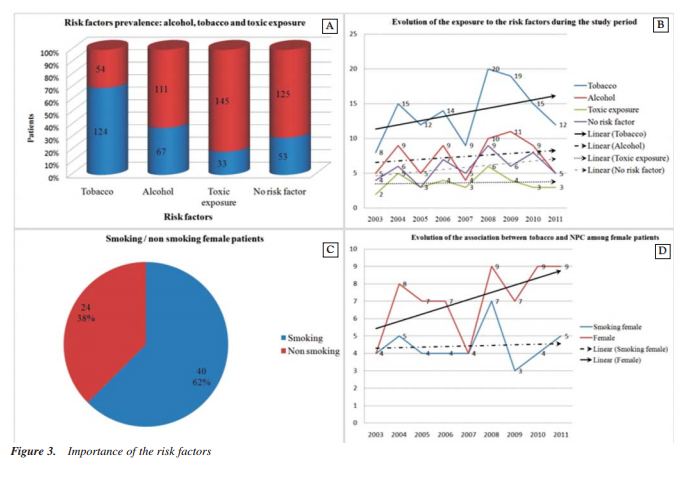
Numerous recent studies have analyzed the connection between the growing number of smoking women and the number of female patients with NPC. According to these studies the number of women with NPC does not grow exponentially along with the number of smoking women. Data obtained by us sustain this general change of perspective which considers that there is a stronger association between NPC and other risk factors than with tobacco use; Fig. 3 C, D. 30 cases out of the total of178 (19 cases with undifferentiated NPC and 11 cases of lymphoma) and belonging to all age groups needed immunological investigation for differential diagnosis. There was a slight male predominance. Theimmunological pattern of our patients presenting withundifferentiated NPC was the following: MNF116, CK19, S100, CD34betaE12, Ki67, EBV positive; the rest of the markers were negative (CerB2, EGFR, COX2, p53, CK7, CD117, VGFR, PCNA, L26/CD20, UHCL1, CD15, CD30, VIM, TTF1, CLA, CK17, CEA, LMP, CD79a, EMA). Concerning the subgroup of patients with lymphoma the immunological pattern included: Ki67, L26/CD20 and EBV positive;other markers were negative (CD79a, Bcl2, CD5, CD10, CLA, UCHL1, MNF116, CD30, VIM, CD23, CyclinD1, Ck34BetaE12, CK19, S100, PAX5, CD3,CD4, CD8). These data support the importance of EBV infection as a risk factor for NPC.
Conclusions
The 178 patients diagnosed with NPC at Coltea Clinical Hospital presented numerous characteristics that sustain the epidemiological data recognized by the international forums such as sex distribution, age groups distribution, histological type distribution and a similar impact of the traditional risk factors.
However there are some specific characteristics for our study group:
- There is a higher number of cases aged over 60 years than younger patients;
- A linear drop in case number for the 30-39 age group;
- A higher number of cases associated with lymphomas;
- A linear drop in case number with spindle cell NPC despite the general rising pattern for all histological types;
- A very large number of cases without any of the traditional risk factors;
- The number of women affected by NPC did not follow the growing number of smoking women;
- The general immunological pattern of our NPC patients was the following: MNF116, CK19, S100, CD34betaE12, Ki67, EBV positive; the restof the markers were negative (CerB2, EGFR, COX2, p53, CK7, CD117, VGFR, PCNA, L26/CD20, UHCL1,CD15, CD30, VIM, TTF1, CLA, CK17, CEA, LMP, CD79a, EMA).
Due to the fact that NPC does not benefit from a national prevention program we hope that this study will draw the attention of other ENT clinics in Bucharest in order tostudy a larger group of patients.
References
1. Chan AT. Nasopharyngeal carcinoma. Ann Oncol. 2010;21 Suppl 7:vii308-12.
2. Guo Y, Chen JX, Yang S, Fu XP, Zhang Z, Chen KH, et al.
Selection of reliable reference genes for gene expression study in nasopharyngeal carcinoma. Acta Pharmacol Sin. 2010; 31(11):1487-94.
3. Qin HD, Shugart YY, Bei JX, Pan QH, Chen L, Feng QS, et al. Comprehensive pathway-based association study of DNA repair gene variants and the risk of nasopharyngeal carcinoma. Cancer Res. 2011;71(8):3000-8. Epub 2011 Mar 2.
4. Cao SM, Liu Z, Jia WH, Huang QH, Liu Q, Guo X, et al.
Fluctuations of epstein-barr virus serological antibodies and risk for nasopharyngeal carcinoma: a prospective screening study with a 20-year follow-up. PLoS One. 2011;6(4): e19100.
5. Yu KJ, Hsu WL, Pfeiffer RM, Chiang CJ, Wang CP, Lou PJ, et al. Prognostic utility of anti-EBV antibody testing for defining NPC risk among individuals from high-risk NPC families. Clin Cancer Res. 2011;17(7):1906-14. Epub 2011 Mar 29.
6. Lee AW, Foo W, Mang O, Sze WM, Chappell R, Lau WH, et al. Changing epidemiology of nasopharyngeal carcinoma in Hong Kong over a 20-year period (1980-99): an encouraging reduction in both incidence and mortality. Int J Cancer. 2003; 103(5):680-5.
7. Adham M, Kurniawan AN, Muhtadi AI, Roezin A, Hermani B, Gondhowiardjo S, et al. Nasopharyngeal carcinoma in Indonesia: epidemiology, incidence, signs, and symptoms at presentation. Chin J Cancer. 2012;31(4):185-96. doi: 10.5732 /cjc.011.10328. Epub 2012 Feb 7.
8. Hsu WL, Yu KJ, Chien YC, Chiang CJ, Cheng YJ, Chen JY, et al. Familial tendency and risk of nasopharyngeal carcinoma in Taiwan: effects of covariates on risk. Am J Epidemiol. 2011; 173(3):292-9. Epub 2010 Dec 10.
9. Thompson CM, Grafström RC. Commentary: mechanistic considerations for associations between formaldehyde exposure and nasopharyngeal carcinoma. Environ Health. 2009;8:53.
10. Golden R. Identifying an indoor air exposure limit for formaldehyde considering both irritation and cancer hazards. Crit Rev Toxicol. 2011;41(8):672-721. Epub 2011 Jun 2.
11. Jia WH, Luo XY, Feng BJ, Ruan HL, Bei JX, Liu WS, et al.
Traditional Cantonese diet and nasopharyngeal carcinoma risk: a large-scale case-control study in Guangdong, China. BMC Cancer. 2010;10:446.
12. Barnes L, Evenson JW, Reichart P, Sidransky D. (Eds): WHO Classification of Tumors. Pathology and Genetics of Head and Neck Tumors. IARC PRESS: Lyon 2005.
13. Anghel I, Greacu IA. Carcinomul nazofaringian. Bucureæti: Ed. Universitas Company; 2002
14. Andrew FO. Epidemiology, Pathogenesis, and prevention of head and neck cancers. Springer: London 2010.
15. Montgomery PQ, Rhys Evans PH, Gullane PJ. Principles and practice of head and neck surgery and oncology 2nd ed. Informa Healthcare: London 2009.
16. Bernier J. Head and Neck cancer multimodality management. Springer: New York 2011.
17. Lu JJ, Cooper JS, Lee AWM. Nasopaharingeal cancer multidisciplinary management. Springer: Heilderberg 2010.
18. Tamiolakis D, Chimona TS, Proimos E, Georgiou G, Perogamvrakis G, Papadakis CE. Neck nodal metastases from unknown primary: cases series. Chirurgia (Bucur). 2008; 103(3):331-5.
19. Anghel I, Anghel AG. Reconstructive rhinoplasty in cases with basal cell carcinoma of the nose. Chirurgia (Bucur). 2012; 107(3):373-8.
20. Berteşteanu SV, Popescu CR, Grigore R, Popescu B. Pharyngoesophageal junction neoplasia--therapeutic management. Chirurgia (Bucur). 2012;107(1):33-8.