I. Anghel, A.G. Anghel
I. Rezumat
Rinoplastia reconstructivã în cazuri cu carcinom bazo-celular nazal
Carcinomul bazocelular este cel mai obisnuit tip de cancer al pielii, 85% fiind localizat în zona capului æi gâtului din care
30% la nivelul piramidei nazale. Autorul prezintã un studiu retrospectiv, propria experienåã, privind tratamentul chirurgical
pe un lot de 31 cazuri cu carcinoma bazocelular de piramidã nazalã, operate în perioada 2006-2011. Partea anatomicã nazalã cea mai frecvent interesatã a fost zona alarã, 58%, urmatã de lobul 18%, perete lateral 12%, dorsum nazal 9% æi 3% basalioma terebrans. În toate cazurile din acest studiu s-a practicat repararea defectelor tumorale cutanate ale nasului utilizând variate lambouri cutanate locale, grefe libere de cartilaj septal æi auricular precum æi grefe libere compuse (piele + cartilaj) din conca æi marginea helixului. Metodele de tratament au depins de localizarea extensiei tumoralã. Cea mai bunã optiune de tratament în carcinomul bazocelular nazal a fost excizia tumoralã radicalã cu margine de siguranåã urmatã de rinoplastie reconstructivã.
Cuvinte cheie: carcinoma bazocelular, rinoplastie reconstructivã, lambou cutanat local, lambou liber compus
ENT Clinic “Coltea”Hospital, University of Medicine “Carol Davila” Bucharest, Romania
Abstract
Basal Cell Carcinoma (BCC) is the most common type of skin cancer, 85% of BCC are located in the head and neck area, of which 30% on the nose. The author present a retrospective study, own experience in surgical treatment in 31 cases with basal cell carcinoma of the nose operated in the period 2005- 2011. The age of patients was between 50 to 90 years old. The anatomical site of the nose the most frecvently involved was ala 58%, and followed of the nasal tip 18%, lateral nose wall 12%, dorsum 9% and 3% basalioma terebrans. In all of the cases in this study it was performed the repair of the skin tumour defects of the nose, using varied local skin flaps, septal and auricle cartilage free grafts and composite graft (skin + cartilage) of conchal and helical rim. Treatment methods were depend on the tumor localization and extension. The best treatment option in BCC of the nose was radical surgical excision whith safety margin of the tumour, followed ofreconstructive rhinoplasty.
Introduction
Basal cell carcinoma is the most common type of skin cancer, it occurs more often in men than in women (1). It is seen more often after age of 50, but in patients younger than 35 it is more aggressive (2). 85% of BCC are located in the head and neck area, of which 30% occurs on the nose (3-4).
Basal cell carcinoma arises in basal keratinocytes in the deep layer of the epidermis (5). This carcinoma grows by direct extension, it does not. blood vessels or lymphatics metastasize.
The evolution may be slowly or rapidly (5-6). The most common risk factors of BCC are (5):
- chronic sun exposure: UVA and UVB radiations, 85% occur on the face and neck;
- repeated sunburns;
- ionizing radiation for acne;
- HIV dieses;
- scared;
- rare gernetic dieses-xeroderma pigmentosa;
Sunlight with ultraviolet light may causing prematureskin aging or skin cancer (5). The sun gives 3 types of ultraviolet radiation:
- UVC radiation 100-290nm, completely absorbed by the ozone layer and does not affect the skin;
- UVB radiation affects the epidermis and is the main agent responsible for sun burns.
- UVA radiation penetrates deeper in to the skin and work efficiently.
Both UVA and UVB radiation can cause skin damage (5): wrinkles, lawered immunity against infection, aging skin desorders and cancer. The possible mecanisms for UV skin demage are collagen breakdown in the dermis, the formation of free radicals, interfering with DNA repair (ensime T4 endonuclease N5) and inhibiting the immune system.
Diagnosis of basal cell carcinoma is done of histopathologycal exam. The preferred type of biopsy depends on the extend of the skin cancer (5,6,7):
- biopsy suspicious looking lesion;
- excise the complete tumor;
There are many treatment options which depend on the location and size of the defect, finally the outcome to be aesthetically and functionally satisfying for the patient: electrodessication and curettage for smaller tumours, excision with plastic reconstruction of the tissue deffect, Mohs’ micrographic surgery, radiation therapy, and cryoterapy (8-13).
The bilobed nasal flap is a useful technique for reconstructing defects of the nose following removal of basal-cell cancers, and it consist of two lobes of skin and subcutaneous tissue based on a common pedicle.V-Y flap is used in dorsum reconstruction in lateral nostril and for small defects of the ala nasi. Nasolabial and cheek skin flap is the ideal sources for partial nasal reconstruction and can be used for coverage of defects of any part of the nose.
Zygomatic flap is used for reconstruction of the lip and nose, especially of the tip and columella.Axial paramedian forehead flap is the donor tissue of choise for nasal reconstruction.
Material and Methods Material and Methods
It is a retrospective study, own experience, in 31 cases with
Reconstructive Rhinoplasty, performed for basal cell carcinoma in the period 2005-2011, in ENT Clinic “Coltea”Hospital, Bucharest. The patients were between 50 and 90 years old. 20 cases were male and 11 were female. 23 patients had a biopsy
–proven basal cell carcinoma a the time of presentation in clinic and in 8 cases the diagnosis was confirmed after surgery using histopathological exam.
The author performed Recostructive Rhinoplasty, using varied local skin flaps in 19 cases, free cartilage graft (septum nasal or auricle) as support for local skin flaps in 4 cases, composite graft (skin and cartilage) ofconcha and helical rim in 6 cases, and in 1 case with recurrent invasive basal cell carcinoma to face and left eye (basiloma or ulcus terebrans) it is used musculocutaneus free flap.
Results
There were 31 tumours (BCC), 20 cases were male, 21 caseswere female.
T he average was 70 years with a range of 50 to 90 years.
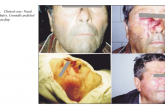
Tumours presentation was following (Fig. 1):
- 20 of the tumours were new presentation (64, 5%);
- 6 of these tumours were recurrent 19, 4%);
- 3 were residual (9, 6 %) after previous excision: simple excision with classic surgery or electro-laser surgery or mohs’micrografic surgery;
- 2 cases were radiorecurrent (6, 5%)
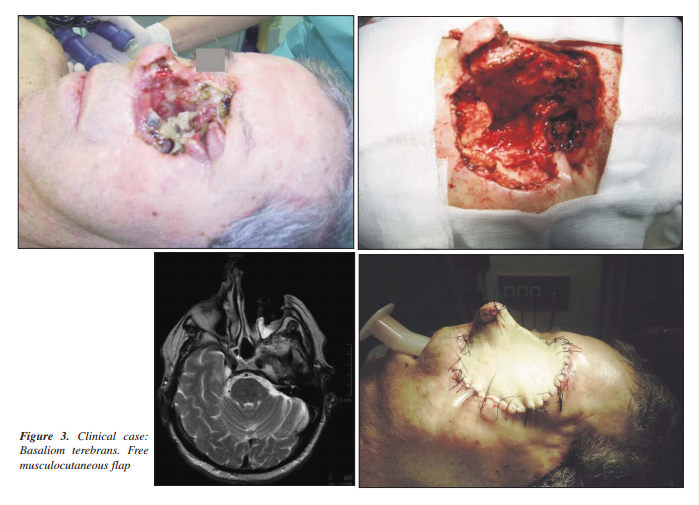
In 1 case with recurrence after 10 years of first - surgery expend invasive rapidly to face and left eye (basalioma or ulcus terebrans).
In this study the anatomic distribution (Fig. 2) of nose carcinomas was the most frecvent the nasal ala 18 cases (58%)
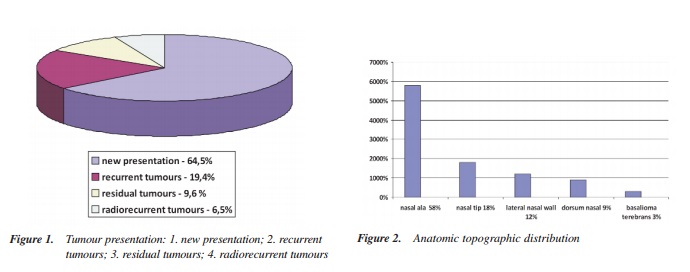
nasal tip 5 cases (18%), lateral nose wall 4 cases (12%), dorsum 3 cases (9%) 1 case basalioma terebrans (3%) invasive in the left midface and eye.
The surgical approach in basal cell carcinoma of the nose consist in excise of tumor in safety tissue margin from 0, 5 to 1 cm.
In 22 cases the safety tissue margin were more than 0, 5 cm, in 9 cases were less than 0, 5 cm, and in the case with
basalioma terebrans was 1cm extended to midface, and left orbital exenteration.
Reconstructive tehniques were:
- Local skin flaps (11 cases) have many advantages as they have their own blood supply and heal well. There are best for reconstructing the convex subunits of the nose but they are limited in length and size. Local flaps are subdivided in to advancement flaps (3 cases), rotation flaps (5 cases) and transposition flaps (3 cases), sliding flaps (3 cases), bilobed flaps ( );
- Dorsal nasal flap (3 cases) used to cover a defect of lower third of the nose;
- Nasolabial flap (6cases) used in the alar subunit;
- Paramedian forehead flap (4cases) the best choise for reconstructing major nasal defects;
- Free cartilage grafts, septal (4cases) and conchal bowl (5cases) were the good support for the skin flap in lateral wall and nasal tip reconstructing.
- Free composite grafts (7cases) consist of skin and cartilage;
The conchal bowl (3cases) contains cartilage with a range of contours which can be used to replace most of the parts of the upper and lower lateral cartilage (9).
The composite grafts have been used to correct small defects of the alar margins and the donors site is often helical rim (4 cases) as its contour is similar to the rim of the nostril (8,10,13).
- Rectus abdominis free musculocutaneous (1case) flap was used for reconstructing a orbitomaxilare defect (Fig. 3) in the case maxilectomy and orbital exenteration (9,14).
Discussions
In our study the treatment of basal cell carcinoma was radical surgical excision with histologic control. The radical surgery has psyhosocial consequences for the pacient, after this surgery resulting the loss of facial function and aesthetic integrity. The facial plastic and reconstructive surgery contribut to correct this loss, the patients have after surgery an acceptable quality of life for several years an outcome aesthetically and functionally, satisfying for the pacient.
Repair of defects of proximal and intermediate parts of nasal dorsum and nasal sidewall
For small defects of the nose was used flaps (advancement, sliding, transposition and rotation flaps), harverseted from nasal skin, forehead and ckeek. Glabela flap used for defects in the intermediate and caudal nasal dorsum (6,11). The paramedian forehead flap was used in large and nasal tip defects.
For nasal sidewall defects a good choise was (Fig. 4) a cranially pedicled nasogenian flap (8,10).
Repair of defects of distal parts of nasal sidewall and nasal wing
Most used was the caudally pedicled nasogenian flap with or without free septal and conchal support cartilage graft (Fig. 5, 6, 7). In cases with defects to all layers of the nasal wing (skin, cartilage )was used composite graft from helical rim
(Fig. 8) and concha (9). The secondary defect at the donor site was closed by a retroauriculary pedicled island flap. Forehead flap was used to correct defects of nasal tip and columella (6,11).
Possible secondary corrections are performed after 6 month post-operator by the patients with stable wound and not
recurrence.
Conclusions
- Basal cell carcinoma is the most common type of the skin cancer in malingnant tumoral pathologie of the
nose;
- It spreads locally and does not metastasize;
- It grows very slowly but in condition with incorrect treatment, after a period can expand rapidly to the
midface, eye (basalioma tenebrans);
- The most frecvernt location for BCC was the nasal ala;
- In this study the majority of the tumours were new
presentations;
- Treatment options depend from the tumor location and extension. The therapeutic success or failure : to have or
not a safety margin when excise the tumour.
- Of choise in nasal BCC is the radical surgical excision.
Facial plastic and reconstructive surgery correct with good results the loss of facial function and aesthetic integrity after radical surgical excision.
The good aesthetic and functional outcome offer an acceptable quality of patients life for several years.
References References
1. Cottel WI. Skin tumors I: basal celland squamous cell carcinoma. Sel Readings Plast Surg. 1992;7(6):1-34.
2. Conley J. Cancer of the skin of the nose. Ann Otol Rhinol
Laryngol. 1974;83(1):2-8.
3. Shanoff LB, Spira M, Hardy SB. Basal cell carcinoma: a statistical approach to rational management. Plast Reconstr Surg. 1967;39(6):619-24.
4. Roenigk RK, Ratz JL, Bailin PL, Wheeland RG. Trends in the presentation and treatment of basal cell carcinomas. J Dermatol Surg Oncol. 1986;12(8):860-5.
5. Brrannon H. About com. Guide. Dermatology, Updated. 2008.
6. Baker R. S Local flaps in facial reconstruction, second edition. Mosby; 2007. p. 71-213.
7. Baker SR, Swanson NA. Management of nasal cutaneous malignant neoplasms. An interdisciplinary approach. Arch
Otolaryngol. 1983;109(7):473-9.
8. Lunatschek C, Schwipper V, Scheithauer M. Soft tissue reconstruction of the nose. Facial Plast Surg. 2011;27(3):249-57. Epub 2011 May 12.
9. Matarasso A, Strauch B. Bilobed nasal skin flaps, vol. 1. In: Grabb’s. Enciclopedia of flaps head and neck, third edition. Ed. Lippincott; 2009. p. 99-101.
10. Frederikr WB, Myers NE. Operative Otolaringology, Head and Neak Surgery. Ed. Saunders; 2008.
11. Roenigk RK. Excision, Dermatologic Surgery, Second Edition. New York-Basel: Dekker Inc.; 1996.
12. Schwipper V. Invasive basal cell carcinoma of the head and neck (basalioma terebrans). Facial Plast Surg. 2011;27(3):258-65. Epub 2011 May 12.
13. Anghel I. Using of facial skin flaps in surgery of nose carcinomas. Otorinolaringologia. 2000;23(1-2):80-83.
14. Albu S, Florian I, Szabo I, Barcut G. Craniofacial resection in malignant neoplasms of the nose and paranasal sinuses.
Chirurgia (Bucur). 2011;106(2):219-225.